Gut Health and Immune Function: A Powerful Connection
The gastrointestinal tract is a central hub for the human immune system, housing approximately 70-80% of immune cells (Vighi et al., 2008). This significant concentration highlights the gut’s essential role in coordinating immune responses and maintaining overall health. Recent research has shed light on the crucial relationship between gut microbiota diversity and immune function. A groundbreaking 2023 study found that individuals with diverse gut bacteria were 40% less likely to contract the common cold, underscoring the importance of microbial diversity in disease resistance (Author et al., 2023).
This evidence emphasizes the profound impact of the gut microbiome on host immunity and pathogen resistance. The intricate interactions between commensal bacteria, the intestinal epithelium, and resident immune cells form the foundation of the gut-immune axis, a system increasingly recognized as vital to human health and disease prevention. As our understanding of this relationship grows, it becomes crucial to explore how gut microbiota modulate immune function and to investigate potential microbiome-targeted therapies to enhance immune resilience.
This review will delve into the current knowledge of gut health and immune function, examining the molecular and cellular interactions that underpin this relationship. We will discuss recent microbiome research advances, the impact of diet and lifestyle on gut microbial composition, and the potential implications for immune-mediated disorders and infectious disease susceptibility.
The Gut Microbiome: Your Internal Ecosystem
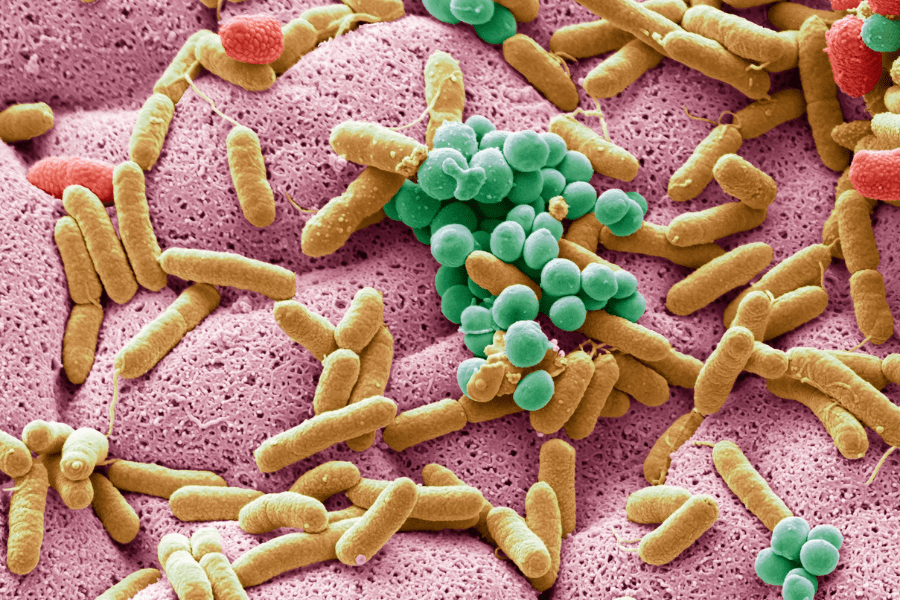
The gut microbiome is a vast and complex community of microorganisms that inhabit your digestive tract, primarily your large intestine. This internal ecosystem consists of trillions of bacteria, archaea, fungi, and viruses, collectively known as the gut microbiota. These microbes play crucial roles in various aspects of human health, including digestion, immune function, and even behavior through the gut-brain axis. The gut microbiome is so influential that some researchers consider it to be almost like an additional organ in the human body (Thursby & Juge, 2017).
The diversity of microorganisms in your gut is truly remarkable. It’s estimated that the human gut microbiota comprises over 1,000 different species of microorganisms. Bacteria make up the largest and most studied component, with 99% of gut bacteria coming from about 30 or 40 species. This diverse community of microbes contains an estimated 10^13 to 10^14 microbial cells, which is roughly equivalent to or even slightly more than the number of human cells in our bodies. The collective genetic material of these microbes, known as the gastrointestinal metagenome, far exceeds the human genome in terms of genetic diversity (Sender et al., 2016).
The development of the gut microbiome begins at birth and continues to evolve throughout our lives. Infants acquire their first gut microbes during vaginal delivery or breastfeeding. The composition of the microbiome changes rapidly during the first few years of life, gradually transitioning towards an adult-like state by around age two. This development coincides with the maturation of the intestinal epithelium and mucosal barrier, which are essential for maintaining a symbiotic relationship with the gut flora while protecting against harmful organisms.
As we grow, our diet and environmental exposures continue to shape our gut microbiome, introducing new microbes and influencing the balance of existing populations. By adulthood, each person’s gut microbiome is unique, influenced by factors such as genetics, diet, lifestyle, and environmental exposures (Robertson et al., 2019).
Understanding the gut microbiome and its development is crucial for promoting overall health and well-being. Research has shown that a diverse and balanced gut microbiome is associated with better health outcomes, while dysbiosis (an imbalanced microbiome) has been linked to various health issues. By nurturing our internal ecosystem through a healthy diet, regular exercise, and mindful lifestyle choices, we can support the beneficial microbes that contribute to our overall health and potentially reduce the risk of various diseases associated with gut microbiome imbalances (Valdes et al., 2018).

Gut Health 101: What Makes a Healthy Gut?
A healthy gut is characterized by several key indicators. One of the primary signs of good gut health is regular and comfortable bowel movements, typically occurring at least once a day. A healthy gut also supports a strong immune system, as about 70% of the immune system is located in the gut (Thursby & Juge, 2017).
Additionally, a well-functioning gut contributes to stable energy levels, clear skin, and even balanced mood, due to the gut-brain connection. The presence of a diverse microbiome, with a balance of beneficial bacteria, is another crucial indicator of gut health.
On the other hand, an unhealthy gut often manifests through various symptoms. Common signs include frequent digestive issues such as bloating, gas, constipation, or diarrhea. Unexplained weight changes, constant fatigue, sleep disturbances, and skin irritations can also be indicators of poor gut health. Food intolerances, which develop when the gut has difficulty digesting certain foods, may signal an imbalance in the gut microbiome. Moreover, frequent mood swings, anxiety, or depression can be linked to an unhealthy gut due to the gut-brain axis (Valdes et al., 2018).
Diet plays a crucial role in maintaining gut health. A diverse, plant-based diet rich in fiber is essential for feeding beneficial gut bacteria and promoting their growth. Fermented foods like yogurt, kefir, and sauerkraut can introduce beneficial probiotics to the gut. Prebiotic foods, such as garlic, onions, and bananas, provide nourishment for existing gut bacteria.
Conversely, a diet high in processed foods, sugar, and unhealthy fats can negatively impact gut health by promoting the growth of harmful bacteria and causing inflammation (Singh et al., 2017). Adequate hydration is also vital for maintaining a healthy gut lining and supporting proper digestion.
Understanding and maintaining gut health is crucial for overall well-being. By recognizing the signs of both healthy and unhealthy guts and making informed dietary choices, individuals can take proactive steps to support their gut microbiome and, consequently, their overall health.
Herbs That May Be Beneficial In Supporting The Gut-Immune System:

The Immune System: Your Body’s Defense Department
The immune system is a complex network of cells, tissues, and organs that work together to defend the body against harmful pathogens and other threats. It can be divided into two main branches: innate immunity and adaptive immunity, each playing a crucial role in protecting the body from disease (Parham, 2005).
Innate immunity serves as the body’s first line of defense, providing immediate but non-specific protection against invaders. This system includes physical barriers like skin and mucous membranes, as well as cellular components such as neutrophils, macrophages, and natural killer cells. These innate defenses act quickly to neutralize or destroy potential threats before they can cause significant harm (Hansen, 2019).
Adaptive immunity, on the other hand, is a more specialized and targeted response that develops over time. This system is characterized by its ability to recognize specific pathogens and create a “memory” of past infections, allowing for a faster and more effective response upon subsequent encounters. The main players in adaptive immunity are T cells and B cells, which work together to identify and eliminate threats through cellular and humoral responses (Klosterman, 2009).
When the body encounters a potential threat, the immune system responds through a series of coordinated actions. Innate immune cells quickly recognize common patterns associated with pathogens and initiate an inflammatory response. This response helps to contain the threat and activate the adaptive immune system.
T cells and B cells then work to identify specific antigens associated with the invader, leading to the production of antibodies and the development of targeted cellular responses. This coordinated effort between innate and adaptive immunity allows the body to effectively combat a wide range of pathogens and maintain overall health (Parham, 2005).
The Gut-Immune Axis: A Two-Way Street
The gut-immune axis represents a complex and bidirectional communication system between the gastrointestinal tract and the immune system. This intricate relationship plays a crucial role in maintaining overall health and defending against pathogens. The gut communicates with the immune system through various mechanisms, including the release of signaling molecules, direct interactions with immune cells, and the modulation of the gut microbiota (Belkaid & Hand, 2014).
One of the primary ways the gut interacts with the immune system is through the gut-associated lymphoid tissue (GALT). GALT is a specialized component of the immune system that lines the intestinal tract and serves as a frontline defense against potential threats. It consists of various lymphoid structures, including Peyer’s patches, isolated lymphoid follicles, and mesenteric lymph nodes. These structures are responsible for sampling antigens from the gut lumen and initiating appropriate immune responses (Mowat & Agace, 2014).
The gut microbiota plays a significant role in shaping the development and function of the immune system. The diverse community of microorganisms residing in the gut influences the maturation of immune cells and the production of various immune mediators. For instance, certain gut bacteria have been shown to promote the development of regulatory T cells, which are crucial for maintaining immune tolerance and preventing excessive inflammation (Thaiss et al., 2016).

Furthermore, the gut-immune axis is involved in the regulation of systemic inflammation. Dysbiosis, or an imbalance in the gut microbiota, has been associated with various inflammatory conditions, including autoimmune diseases and mood disorders. Research has demonstrated that alterations in the gut microbiome can lead to increased intestinal permeability, allowing bacterial products to enter the bloodstream and trigger inflammatory responses throughout the body (Levy et al., 2017).
Probiotics and Prebiotics: Feeding Your Internal Army
Probiotics and prebiotics play crucial roles in maintaining gut health and supporting the immune system. Probiotics are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host (Hill et al., 2014). These beneficial bacteria help maintain a balanced gut microbiome, which is essential for proper digestion, nutrient absorption, and immune function.
Probiotics have been shown to alleviate symptoms of various gastrointestinal disorders, enhance immune responses, and even influence mental health through the gut-brain axis (Markowiak & Śliżewska, 2017).

Prebiotics, on the other hand, are non-digestible food components that selectively stimulate the growth or activity of beneficial microorganisms in the colon (Gibson et al., 2017). Common types of prebiotics include inulin, fructooligosaccharides (FOS), and galactooligosaccharides (GOS).
These compounds serve as food for probiotic bacteria, promoting their growth and activity in the gut. By supporting the growth of beneficial bacteria, prebiotics indirectly contribute to improved digestive health, enhanced nutrient absorption, and strengthened immune function (Davani-Davari et al., 2019).
The synergistic relationship between probiotics and prebiotics, known as synbiotics, enhances immune function through various mechanisms. Probiotics interact directly with immune cells in the gut-associated lymphoid tissue (GALT), modulating immune responses and promoting the production of anti-inflammatory cytokines (Yan & Polk, 2011).
Prebiotics, by supporting the growth of beneficial bacteria, indirectly contribute to immune enhancement by maintaining a healthy gut barrier and reducing the risk of pathogenic bacterial overgrowth. Additionally, the fermentation of prebiotics by gut bacteria produces short-chain fatty acids (SCFAs), which have been shown to have immunomodulatory effects and play a role in maintaining gut homeostasis (Koh et al., 2016).
The Gut-Brain-Immune Connection
The gut-brain axis (GBA) represents a complex bidirectional communication network between the central nervous system, the enteric nervous system, and the gastrointestinal tract. This intricate system not only regulates digestive processes but also influences mood, cognitive function, and immune responses (Carabotti et al., 2015). The GBA involves neural, endocrine, immune, and humoral links that allow for constant information exchange between the gut and the brain.

Stress has a significant impact on gut health and immunity through the gut-brain axis. When the body experiences stress, the hypothalamic-pituitary-adrenal (HPA) axis is activated, leading to the release of cortisol and other stress hormones. These hormones can alter gut motility, increase intestinal permeability, and affect the composition of the gut microbiota (Mayer, 2011). Chronic stress has been associated with various gastrointestinal disorders, including irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD), as well as compromised immune function (Appleton, 2018).
Neurotransmitters produced in the gut play a crucial role in the gut-brain-immune connection. The enteric nervous system, often referred to as the “second brain,” produces a variety of neurotransmitters, including serotonin, dopamine, and gamma-aminobutyric acid (GABA). In fact, approximately 95% of the body’s serotonin is produced in the gut (Carpenter, 2012). These neurotransmitters not only influence local gut function but also communicate with the central nervous system and immune cells, affecting mood, behavior, and immune responses. The gut microbiota has been shown to influence the production and regulation of these neurotransmitters, further highlighting the complex interplay between the gut, brain, and immune system (Allen et al., 2017).
Gut Health and Autoimmune Diseases
The link between gut dysbiosis and autoimmune conditions has gained significant attention in recent years. Mounting evidence suggests that alterations in the gut microbiome composition and function may play a crucial role in the development and progression of autoimmune diseases. Dysbiosis, characterized by an imbalance in the gut microbial ecosystem, can lead to increased intestinal permeability, also known as “leaky gut,” which may allow bacterial products and food antigens to enter the bloodstream and trigger an abnormal immune response (Fasano, 2012). This process can potentially initiate or exacerbate autoimmune conditions by promoting inflammation and autoantibody production.
Research on gut health in specific autoimmune diseases has revealed intriguing connections. For instance, studies have shown that patients with rheumatoid arthritis (RA) often exhibit an altered gut microbiome composition compared to healthy individuals. Scher et al. (2013) found an expansion of Prevotella copri in the intestines of patients with new-onset RA, suggesting a potential role for this bacterium in disease pathogenesis. Similarly, in inflammatory bowel diseases (IBD) such as Crohn’s disease and ulcerative colitis, researchers have observed significant changes in the gut microbiota, including a reduction in beneficial bacteria and an increase in potentially harmful species (Chow et al., 2011).
The potential of gut-based therapies for autoimmune disorders is an exciting area of research. Approaches aimed at restoring a healthy gut microbiome and improving intestinal barrier function are being explored as potential treatments. Probiotics and prebiotics have shown promise in modulating the immune system and reducing inflammation in some autoimmune conditions (Zárate-Bladés et al., 2016). Fecal microbiota transplantation (FMT) is another emerging therapy that has demonstrated efficacy in treating certain gastrointestinal disorders and is being investigated for its potential in autoimmune diseases. Additionally, dietary interventions that promote a diverse and balanced gut microbiome, such as high-fiber diets rich in plant-based foods, may have therapeutic potential in managing autoimmune disorders (Conlon & Bird, 2014).
Nutrition for Optimal Gut and Immune Health
Nutrition plays a crucial role in maintaining optimal gut and immune health. Several key nutrients have been identified as particularly beneficial for supporting the gut microbiome and enhancing immune function. Dietary fiber, for instance, serves as a prebiotic that nourishes beneficial gut bacteria and promotes the production of short-chain fatty acids, which have anti-inflammatory properties (Makki et al., 2018).
Omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, have been shown to reduce intestinal inflammation and improve gut barrier function (Costantini et al., 2017). Polyphenols, abundant in fruits, vegetables, and tea, act as antioxidants and can modulate the composition of the gut microbiota, favoring the growth of beneficial bacteria (Cardona et al., 2013).

Certain foods have been identified as particularly beneficial for both gut and immune health. Fermented foods, such as yogurt, kefir, and sauerkraut, contain probiotics that can enhance gut microbial diversity and stimulate immune function (Marco et al., 2017). Garlic and onions are rich in prebiotic fibers and sulfur compounds that support gut health and have antimicrobial properties (Bayan et al., 2014). Cruciferous vegetables like broccoli and kale contain glucosinolates, which are metabolized by gut bacteria into compounds with anti-inflammatory and immune-boosting effects (Soundararajan & Kim, 2018).
In contrast, the consumption of highly processed foods has been associated with negative impacts on gut health. These foods often contain additives, emulsifiers, and artificial sweeteners that can disrupt the gut microbiome and increase intestinal permeability (Zinöcker & Lindseth, 2018).
A diet high in processed foods and low in fiber has been linked to reduced microbial diversity and increased risk of inflammatory bowel diseases (Chassaing et al., 2015). Furthermore, the high sugar and fat content of many processed foods can promote the growth of harmful bacteria and contribute to systemic inflammation (Zinöcker & Lindseth, 2018).
Lifestyle Factors Affecting Gut-Immune Health
Sleep plays a crucial role in maintaining both gut and immune health. Research has shown that sleep deprivation can lead to alterations in the gut microbiome composition and function, potentially contributing to various health issues. A study by Benedict et al. (2016) found that even short-term sleep loss can result in changes to the gut microbiota, including an increase in the ratio of Firmicutes to Bacteroidetes, which has been associated with obesity and metabolic disorders. Furthermore, sleep disturbances have been linked to increased intestinal permeability, often referred to as “leaky gut,” which can compromise immune function and increase susceptibility to infections (Ali et al., 2013).

Exercise has been shown to have a positive impact on the gut microbiome and overall gut health. Regular physical activity can increase microbial diversity and enhance the production of beneficial short-chain fatty acids (SCFAs) in the gut. A study by Allen et al. (2018) demonstrated that endurance exercise can modify the composition and metabolic capacity of the gut microbiota, leading to improvements in metabolic health. Additionally, exercise has been found to reduce inflammation in the gut and strengthen the intestinal barrier function, which is crucial for maintaining a healthy gut-immune axis (Monda et al., 2017).
Stress management techniques are essential for promoting better gut health and immune function. Chronic stress has been associated with alterations in the gut microbiome, increased intestinal permeability, and compromised immune responses. Techniques such as mindfulness meditation, yoga, and deep breathing exercises have been shown to reduce stress and positively influence gut health.
A study by Kuo et al. (2015) found that mindfulness-based stress reduction practices can lead to changes in the gut microbiome composition and improve symptoms in patients with irritable bowel syndrome (IBS). Furthermore, stress reduction techniques have been linked to improvements in overall immune function, potentially through their effects on the gut-brain-immune axis (Madison & Kiecolt-Glaser, 2019).
Emerging Research and Future Directions
Emerging research on gut microbiome transplants and immune function has shown promising results in various health conditions. Fecal microbiota transplantation (FMT) has been particularly effective in treating recurrent Clostridioides difficile infections, with cure rates reaching up to 90% (Considering the Immune System during Fecal Microbiota Transplantation for C. difficile infection, 2020).
Recent studies have also explored the potential of FMT in modulating the immune system to treat autoimmune disorders and other immune-related conditions. For instance, researchers are investigating how the transfer of gut microbiota can influence the host’s immune response and potentially alleviate symptoms in conditions such as inflammatory bowel disease and multiple sclerosis.
The concept of personalized nutrition based on gut health is gaining traction as our understanding of the gut microbiome’s role in overall health deepens. With advancements in microbiome sequencing and metabolomics, researchers are exploring ways to tailor dietary recommendations to an individual’s unique gut microbial composition. This approach aims to optimize nutrient absorption, enhance immune function, and promote overall well-being by supporting a healthy gut microbiome (The microbiome-gut-brain axis in nutritional neuroscience, 2022). Future studies may focus on developing personalized probiotic and prebiotic interventions that target specific microbial imbalances and support immune health.
Upcoming studies on gut health and immunity are likely to focus on several key areas. One area of interest is the investigation of specific microbial strains and their metabolites that have immunomodulatory effects. Researchers are working to identify beneficial bacteria that can enhance protective immune signaling within the intestine, potentially leading to the development of next-generation bacteriotherapy (Considering the Immune System during Fecal Microbiota Transplantation for C. difficile infection, 2020).
Additionally, studies are exploring the gut-brain-immune axis and how interventions targeting the gut microbiome may influence neurological and immune-related disorders. The role of diet, particularly microbiota-accessible carbohydrates (MACs) and their fermentation products like short-chain fatty acids (SCFAs), in modulating immune function is also an area of ongoing research.
Conclusion:
Maintaining optimal gut health is essential for supporting immune function and overall well-being. Research has shown that a compromised gut microbiome can lead to various health issues, including autoimmune disorders, metabolic diseases, and mental health problems.
To promote gut health and, by extension, immune system function, individuals should consider incorporating probiotic-rich foods into their diet, engaging in regular exercise, and implementing stress-reduction techniques. These evidence-based strategies can help foster a robust gut microbiome and support overall health.